Acknowledgements
The Military Birth Resource Network would like to thank Kelsey Hurlburt, Toni Wenger, Amanda Dodson, Linda Herrick, and Sally Riley for developing and putting this survey together.
We also want to take the time to say thank you to the doulas, providers, and other birth professionals who provided feedback on the responses.
We want to recognize all the military families who took the time to fill out this survey and provided us with responses. Our goal is to start a conversation with the military health system and military family services on where needs are lacking and gaps in care currently exist.
Having a baby is indeed one of the most incredible experiences in one’s life. However, it can also be one of the most stressful. We are a mobile society and frequently do not have close relatives who are able to attend the birth or assist new parents immediately after the birth. From the perspective of the health care system, safety is a top priority as it should be. A frequently heard comment by health care providers is, “A healthy baby and healthy mom is our goal.” From the woman’s point of view however, birth is a life passage, an event in which both safety and satisfaction have great significance. If having a healthy baby and healthy mother were enough, we would not have the high incidence of postpartum depression and mood disorders following a birth experience with a “healthy mom and baby.” Military members and their partners have special circumstances to contend with when having a baby.
In May of 2019 the Military Birth Resource Network created a survey with Resources by Kelsey to get a sense of the pregnancy, birth, and postpartum support experienced by women who received birth-related care on US military installations within the last 10 years.
Edit: In reviewing the data we identified the correct date of the survey was conducted in May 2019 and reported in 2020. We apologize for any misunderstanding.
We surveyed the categories of those with a
Younger/Only Child
Second Youngest/Middle Child
Third Youngest/Next Oldest Child
The Results
We asked everyone if within the past 18 years, if they received any pregnancy, birth, OR postpartum medical OR non-medical care, such as parenting classes, on a United States military installation?
884 responded.
754 (85.3%) said yes. 17 (1.9%) said no. 113 (12.8%) did not receive care on an installation.
Non-medical pregnancy-related care
We asked those with a youngest/only child if they received non-medical pregnancy-related care, such as prenatal classes, on a US military installation?
Out of 725 responses.
374 (51.6%) said YES they received non-medical care. 351 (48.4%) said NO, they did not receive non-medical care.
Of the 725 responses, 509 (70.2%) delivered on a military installation.
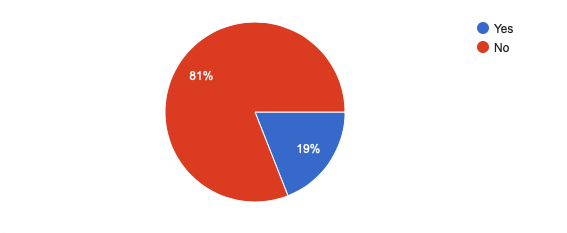
For postpartum care 587 (81%) responded with they did not receive any postpartum-related non-medical care, such as parenting classes, on a US military installation.
Out of the 725 people, 549 did say YES they received a 6 week check up or lactation support, on a US military installation.
Postpartum Depression/Posptartum Anxiety Check Up
Postpartum mood disorders are one of the leading complications of pregnancy, greater than gestational diabetes and gestational hypertension. One in every ten women suffers from a postpartum mood disorder. Symptoms may include the inability to adequately care for oneself or the baby, loss of appetite, depression, anxiety, insomnia, recurrent thoughts of suicide and death, and in some cases complete mental breakdown. Pregnancy and postpartum mood disorders affect not only the mother but the entire family.
A recent military study showed that for a woman whose spouse/partner was serving in the military and was deployed, the rate of postpartum mood disorders was 2.3 times that of the civilian population. Military families are often separated, move frequently, and lack the support essential to decreasing the incidence of pregnancy and postpartum mood disorders. It is very difficult for an individual serving in the military to be “battle ready” when worried about their partner.
Postpartum mood disorders may occur at any time during the first year after the birth. The American College of Obstetricians and Gynecologists, ACOG, has recommended that pediatricians/family practice physicians evaluate the mother for postpartum mood disorders at each child’s routine visit for the first year.
In 2006, Childbirth Connection released a ground-breaking report of the experiences of mothers in the United States in the first 18 months after giving birth called New Mothers Speak Out. Based on results from Childbirth Connection’s national Listening to Mothers II Survey and Listening to Mothers II Postpartum Survey, the report highlights that new mothers in the United States have diverse, demanding responsibilities. They experience notable social, physical, and emotional challenges that frequently persist over many months and they face inadequate policies, services, and support.
Results from this study showed that mothers gave high ratings for their baby’s health but identified many concerns about their own wellbeing. Those included:
Many mothers, especially those with cesarean births, reported that pain interfered with their routine activities and physical problems interfered with the ability to care for their infants.
At 6 months, many women continued to experience stress (43%), sleep loss (34%), physical exhaustion (25%), and lack of physical desire (26%).
Validated mental health screening tools found that at the time of the survey 63% of mothers were likely to be experiencing some degree of depressive symptoms and 18% were experiencing some symptoms of post-traumatic stress related to their childbirth experience.
For those with the only child/youngest category, we received 549 responses when we asked if they were evaluated for postpartum depression (PPD) or postpartum anxiety (PPA) at their 6 week postpartum check up.
While there was a mixed response of those evaluated, 25 said they were diagnosed with PPD and PPA while 41 were diagnosed with PPD and 9 for PPA during the first year of postpartum.
Those evaluated for postpartum depression (PPD) or postpartum anxiety (PPA) at their 6 week postpartum check up.
Those diagnose within the first year of being postpartum.
Were services or classes such as New Parent Support utilized during the pregnancy and postpartum period?
The New Parent Support Program (NPSP) promotes healthy Families through a variety of services including home visits, support groups, and parenting classes. These programs can help service members and their families learn to cope with stress, isolation, post-deployment reunions, and the everyday demands of parenthood. These services are free of charge to families.
Each installation has a unique New Parent Support Program service.
We found that out of the 725 people responding, only 218 (30.1%) utilized these services. Many found the services to be beneficial and easy to access.The majority utilized the prenatal classes and postpartum visits offered by NPSP.
However, out of 507 responses, 275 (54.2%) said they were not aware these services or classes were available.
Centering Pregnancy
Centering Pregnancy is a 10-session prenatal care model conducted in a small group setting. Centering Pregnancy® is better care with a team approach to care that actively engages patients in goal setting, skill-building, and peer support. Provider facilitated group health care allows more time to explore important health topics. The model includes three components of care: assessment, learning, and community building.
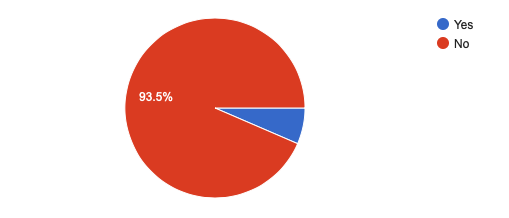
Out of 725 responses, 678 (93.5%) did not utilize an installation Centering Pregnancy® during their pregnancy.
Of the 678, 373 (55%) said they were not aware if their installation offered these services or not.
Was Centering Pregnancy utilized?
55% were not aware of centering pregnancy being available or not.
Lactation Support
As we continued with the youngest/only child group we asked if a lactation consultant connected to a US military installation was utilized at any point during pregnancy or postpartum?
369 (50.9%) of the 725 responded no, while 356 (49.1%) said yes.
We also found that lactation support was mostly utilized within the first 48 hours after birth.
Doula Support
Doulas provide support with statistics showing many benefits of bettering outcomes. Doulas are not medical personnel who rely on excessive technology, they rely instead on more well-tested and traditional methods of pregnancy and labor support. This care results in significant costs savings, improved health for mother and baby, decreased postpartum mood disorders, and significant improvement in both the immediate and long-term dynamics of the family.
Of the 725 responses, 149 (20.6%) said they utilized a doula. With a high number of those finding the emotional support being the most beneficial during labor. Labor and delivery education, physical support during labor and emotional support during pregnancy were also valuable responses from mothers.
Other Factors
Deployments and PCS’ing can also play a role in how families feel supported and what types of resources they have access too.
229 (31.6%) responded that they had a spouse deploy during pregnancy, while giving birth, or within the first year postpartum.
Of those 229, only 13 (5.7%) were offered any additional support services.
Had a spouse deployed during pregnancy, while giving birth or first year postpartum.
Moved during pregnancy
162 (22.3%) Moved, 563 (77.7%) Did not move.
Subsequent children
Second Youngest/Middle Child
Third Youngest/Next Oldest Child
As we continued the survey for those with a second and third child, findings were similar. 412 of the the 887 had a second child and 134 had a third child. The findings from delivering on base to utilizing a doula were similar. Many did not know base programs existed or when they did, the survey showed it was primarily prenatal classes and postpartum home visits being utilized.
Future Care
Okinawa, Japan serves as an example of the lack of support for birthing mothers and their families. Despite programs that the military currently provides, there are serious gaps in family support. U.S. Naval Hospital Okinawa delivers on average 100 babies a month. Women are being sent home with minimal or no breastfeeding knowledge or support. Secondary caregivers now receive up to two weeks of leave in the Marine Corps and Navy, and three weeks in the Air Force and Army. Not all families cannot afford to bring other family members to Japan to provide support. This can result in increases of traumatic births experiences, postpartum depression, mood disorders and breastfeeding problems.
Despite the excellent care provided at U.S. Naval Hospital Okinawa, it does not replace the one-to-one support that military wives/partners need before, during, and after their pregnancies. These families are placed in unfamiliar situations, rather than being the supported at such a critical time in their lives. Additionally, COVID continues to complicate traveling overseas, thus resulting in another consideration of limiting support for families. Many Military Treatment Facilities have stopped allowing doulas as a second support person.
While U.S. Naval Hospital Okinawa serves as one example, this is happening at duty stations CONUS and OCONUS. We not only owe our active duty members the best of care, we also owe it to their families.
We asked everyone if they were to become pregnant again, how likely is it that they would choose to utilize US military installation medical care for the pregnancy?
838 people responded. We rated from 1 -7. 1 being the very unlikely to 7 being the very likely. These responses were insightful.
320 (38.2%) said it would be very unlikely to seek future medical care on a US military installation.
170 (20.3%) said they would very likely seek future medical care on a US military installation.
Will future medical care be sought on a US military installation?
We also asked how likely would be to choose to utilize a doula for pregnancy, birth, and/or postpartum care?
292 (34.8%) said it was very likely
187 (22.3%) said it was very unlikely
Would a doula be utilized?
The Demographics
838 Responses
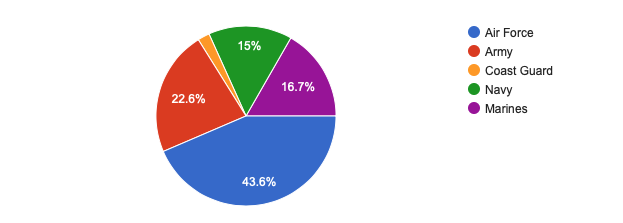
Branch of Service affiliation
Military Status
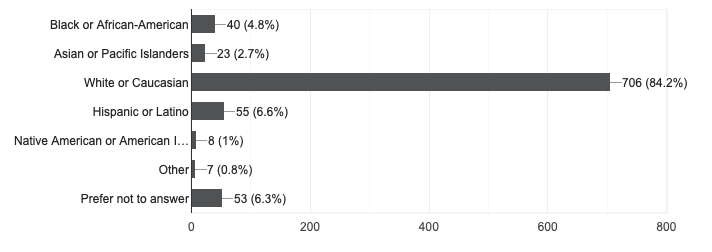
Racial or ethnic group(s) identified
The mission of MBRN is to support healthy, safe, and satisfying pregnancies, births, and postpartum experiences for military families across the globe. Evidence-based information as well as resources that connect families with professionals in the military community who practice evidence-based care. The Military Birth Resource Network wholeheartedly believes this type of information and support is critical to empowering families to create a satisfying and healthy birth environment for their family. It is MBRN’s goal to encourage a celebration of birth throughout military communities by building awareness of the profound impact of mother-centered maternity care and support. MBRN currently has chapters that provide doula services and promote health education and support for prospective families in England, Germany, Japan, and at multiple military installations in the United States.
Comments regarding any of your pregnancy, birth, or postpartum experiences on a US military installation.
Experience with Doulas
- I am very nervous to deliver at my current installation. They have no NICU and very limited support. I am overseas and cannot just go off base for care as I would like. I will say though that the OBs here have been very caring helping me through a miscarriage. I would like more access to a doula or midwife here are well if I get lucky to have another pregnancy.
- With my second/middle child. I started at SHAPE but husband was stationed next to Korea. So I went to Utah to be close with family. Setting up an obgyn was tricky as I want bear a military installation. The closest one was 1 1/2hrs away. Finding a pediatric Dr was also difficult to set up through Tricare. But once that was done. I found civilian doula, and local birthing class, and the Tricare nurse did call in occasion while I was pregnant to check up on me.
- My first experience at Portsmouth in 2003 was miserable. I was a young active duty officer and felt horribly intimidated. The saving grace was my kind female OB/GYN. My successive experiences in Newport and Mayport/Jacksonville were much better, but I was older and experienced. My doulas were wonderful and I feel all first time mothers, particularly hyper stressed military spouses, should have a doula. They were a blessing to both me and my husband.
Base Programs
- I knew there was new parent support with my last, but I wasn’t unable attend any of them. I was told I was not alllwed to bring other kids just the baby, so I couldn’t attend since I have more children. I guess the base programs are only meant for first time moms.
- It's great that all these programs are available on base, but they need to be advertised more. I didn't find out about any of them until after I would have been able to use them. Also, maybe having a briefing of sorts on how commanders should handle members of their squadron starting a family. No pregnant woman should be told that she's a distraction to her husband just because she's having a baby.
- I really loved my New parent support nurse with my first (2016), I didn’t NOT appreciate her contracted being cut on short notice. I didn’t have the time to say good bye to her. She was a vital part to my PPD support (that I didn’t know I had). After I was notified she was fired, I didn’t ask for a replacement. This was not healthy to all the mothers she was seeing. When I had my second, I welcome a NPSN but it was not the same. But did give me something to look forward to.
- I wish there was a check in with your medical team before the 6 week check up for the mother. There was a huge disconnect from giving birth at the hospital and 6 weeks later. Thankfully new parent support stepped in to help.
- Any post partum classes suggested didn't allow me to bring my 2 yr old &4yr old. I was still new to the area and didn't have many friends so this isolated me even more.
- Other than a 1 day parenting class, there isn’t any support for expecting mom’s on post. We have to see an German ob, who don’t really explain things and we have little knowledge of what we’re supposed to do. I wish there was a birthing class on post like at the military hospitals back in the states and just more support on the military side. It’s scary having a baby the first time and having your first child overseas is even scarier.
- After PSCing to Okinawa at 23 weeks gestation, all the military hospital prenatal birth and breastfeeding classes were full. I was told they would not be offering any more before my due date. I found this unbelievable especially during the height of PCS season to offer nothing to moms arriving. Also the only LC at the hospital made it very clear at support groups that if a mother wasn't willing to give up dairy there wasn't much more she could help you with…not helpful or backed by science.
Military Treatment Facility Care
- I tried for over 6 weeks to do centering however was denied even though my husband was deployed my entire pregnancy, missing the birth of our first child. OB/GYN was over populated. I had difficulty making appointments and was told “you’re lucky you even got the appointment you did” Even though it was 2 weeks later than what I was suppose to be seen in my third trimester. At one appointment, there was no chart review completed because the doctor thought I was someone else. They had cancelled two of my appointments with out bringing it to my attention. My postpartum check up did not happen until I was 10+ weeks post partum even though, I had complications with healing process. 2 weeks post partum I tore 1 of the stitches. I did enjoy the L&D department. They were organized and professional. I would like to add I was not educated on a doula. I would have been very interested in that option since I had no family present during delivery and husband was deployed.
- While my delivery did not go as planned, I had wonderful care through all stages of my pregnancy, delivery, and postpartum. All of the midwives I saw before and after were wonderful, caring, and attentive.
- Military members and dependents need personalized medical care especially during pregnancy. Midwives would be a great addition. Lactation consultants need to be more up to date with current breastfeeding information and resources.
- We delivered 2 of our 5 kiddos on bases. Off base beats those experiences on most points. Having said that, we were always thankful of our care on base as a whole over the course of my 18 years and my husbands 20 years with the Air Force. Sometimes you have to demand care, but as you learn to navigate the system, you find it an amazing benefit of Service.
- Ive pcsd during 2 pregnancies and each time it was very difficult to establish care ON THE MILITARY side. Weve only been on smaller bases that did not offer hospitals and each time to get a referral to an outside obgyn took a ridiculous amount of time. I was 30+ weeks pregnant having to find time to go on to base to do a blood test or pee to prove I was pregnant and had to have hard copies of all my paperwork from our last I installation to take into my doc. Luckily the civilian docs just needed the paperwork and didnt submit any insurance claims until after the referals went through so i qas able to receive care because each time it took over a month for the referal process and id have missed multiple appointments and was considered high risk thanks to having HG.
- Prenatal care at MCAS Iwakuni is extremely lacking. When we relocated here in 2017, I was 12 weeks pregnant and a birthing center was supposed to already be open (for the first time) on this base. It did not open, and our options were travel by a 6-hour train at 36 weeks to deliver and then travel 6-hour return with newborn days after delivery or deliver in a Japanese “hospital” with very minimal (or none) English-speaking staff without a translator. Because we had pets and could not leave them for a month, we chose to deliver in the Japanese hospital. Although for me my experience ended up being alright (in that I was fine and had a healthy baby), I did have some complications and it was very scary and a cause for anxiety at times. After I gave birth, our clinic did open-briefly. It was closed down 2-3 weeks after opening because they found their sterile equipment for c-sections was contaminated. They never communicated this to anyone who had c-sections in that short amount of time—these women actually found out on social media. We have still yet to be informed on exactly why the issues have not been fixed and how long it will be until they are resolved. This was approximately a year ago, and it is still closed. I am now pregnant again, sue this June, and again have the same two options. There is no arranged childcare at the base 6 hours away, so again it is really not a feasible option for us (or many others). Again I will have to deliver in a Japanese hospital. My prenatal care on base has been mostly adequate, however basic things like a urine screening at each visit (that is a simple standard of care in civilian practices) are not performed. To say that I have been extremely disappointed in our medical care here, both throughout pregnancy and postpartum, would be an understatement. I am filling this out in hopes that someone can make a difference and help the women stationed here at MCAS Iwakuni with the medical injustices they have to bear on a daily basis.
- Childcare would be so helpful. With my 2nd and 3rd child, my spouse was deployed for a portion of those pregnancies and postpartem, and sometimes it was very difficult or impossible to get to any prenatal classes or appointments. Childcare for my older children would have been very helpful.
Better Lactation Support
- No lactation consultant at Fort Bliss. I had to pay for or us free resources out in the community.
- Better support for breastfeeding mothers. Lack of time/facilities to pump made continued breast feeding for more than a few months incredibly difficult. Lack of understanding that for some mothers 20 minutes to set up, pump and cleanup is just not feasible.
- As an active duty shift worker, finding the time to pump for my infant was extremely difficult. Additionally, there were no designated pumping rooms that were in good working order. I had to pump in an empty room and sometimes that was impossible because all the rooms were taken by patients. At some point I just gave up which really broke me because I wanted to breastfeed exclusively for a year. I made it until I went back to work. Additionally, childcare is an issue. There are not nearly enough childcare options that support shift workers, especially for single parents such as myself. I have to spend a significant amount of my money on the CDC and supplemental care which has led to my bank account being overdrawn multiple times. I have had to jump through hoops last minute to find care because sitters are not reliable, and while I was waiting to start at the CDC last year, my then three month old was abused by his babysitter. FCC providers do not have the availability that they advertise, and that’s only if they even respond to my inquiries to begin with. I do not expect to receive perks as I am active duty, however, childcare and ensuring my child is safe is a major priority for me, one that has such an impact on my life that it has made me consider separating, despite wanting to do 20 years; I’m at 2.5 years right now.
- Lactation support in 2013 at JBLM was very difficult to access, and was only offered during your hospital stay and during group lactation sessions. My oldest never wound up latching and I had to exclusively pump for over a year. With my second child (all civilian services), I was able to get individual appointments with a lactation consultant weekly through her pediatrician and wound up working through her latching issues.
- Mom2Mom support group meet ups literally saved my sanity and my life during my postpartum. Amy Goodenow (LC) on our base was incredibly influential in my breastfeeding journey. The prenatal classes (mom and das boot camp, and breastfeeding 101) were SO helpful for me.
- Disliked the emphasis on group sessions. There was NO access to lactation consultant at all. The staff was not well trained to assist new mothers and unable to answer questions about breastfeeding.
- I was very fortunate to be well-educated with plenty of experience in perinatal nursing before having my own very high risk twin pregnancy w/premature delivery while dual active duty, or my babies’ outcomes may have been very different. It is unfortunate that military hospitals have jumped on the BFHI bandwagon, as their clientele is disadvantaged in a variety of aspects as noted above. The BFHI does a terrible disservice to birthing people and their babies by pushing exclusive breastfeeding at all costs. Rates of infant falls, Sudden Unexpected Postnatal Collapse (SUPC), hypoglycemia causing decreased academic potential in longitudinal studies, and readmissions for dehydration/jaundice/failure to thrive have all increased since BFHI implementation. There is also a wide range of inconsistent information given by healthcare providers d/t the push for EBF at all costs. On the other hand, the Fed is Best Foundation has excellent EBP guidelines and medical/community support for parents to feed their children in the way that best facilitates neonatal/pediatric physiologic health and parental mental health.
Other Comments about Options, PPD and Centering
- Tricare should allow for more birthing options in ALL regions ie Birthing Centers and Home Births. There should be more prenatal classes geared toward labor and birth and coping with delivery not how to just care for a newborn. There should be lactation consultants that can do home visits. Infants should be evaluated for lip and tongue ties at birth by someone trained to identify them.
- As a home birthing mom, I felt the military held that against me. While active duty I was looked down on by my CoC for having a home birth. We need to bring the military up to speed on birth options.
- I thought Landstuhl took good care of us. I wish I had stayed a day or two longer but otherwise it was great care. I think the PPD questionaires are way too focused on one particular problem which is bonding with the baby. For example, I bonded well with the baby but everyone else around me made me feel depressed and anxios. I didn't feel like there was a person there that I would have trusted to talk to about this. Access to a counselor specifically focused on pregnancy and birth may be a better idea.
- Overwhelming and not enough info given to newly pregnant first time moms prior to joining Centering or having appointments. Would be good to have a packet of information handed to every woman confirming pregnancy and out everything offered and options for appointments or signing up for Centering. They had fluers on the desk for Centering that I just happen to see... If I did not see them myself I would have never known about it and it was so much more attentive than regular appointments would have been. I also had to call twice to make sure they put me in the class. Organization needs fixing. Also... Give moms 10 minutes to relax before taking blood pressure in appointments. They always said they would give us a few but then rushed us to take it. I was wrongly thrown into the maternal fetal medicine clinic due to two high readings which never continued.